Houston innovator powers health care innovation by collaboration — inside and outside of the hospital setting
HOUSTON INNOVATORS PODCAST EPISODE 202
It might surprise most to know that Houston Methodist doesn't have an innovation department within their hospital system — at least not one set up as you'd imagine, with a team specifically dedicated to innovation. Instead, Houston Methodist's Digital Innovation Obsessed People, or DIOP, consists of leaders across departments.
Michelle Stansbury is one of those leaders. As vice president of innovation and IT applications at Houston Methodist, she oversees the system's IT department and serves as a leader within its innovation efforts. This includes the Center for Innovation Technology Hub — which opened in 2020 in the Texas Medical Center location and opened its Ion outpost last week.
Stansbury explains on the Houston Innovators Podcast how effective this distribution of innovation responsibilities has been for Houston Methodist. With everyone having a seat at the table — operations knows the biggest problems that need solutions, IT knows how to deploy technology, etc. — implementation of new innovations has been sped up.
"If we partner together, we should be able to succeed fast or fail fast," she says on the show. "We've been able to find a solution, pilot it, and, if it works well, roll it out at a speed that most other organizations have not been able to do. It's been highly successful for us."
The newest way Houston Methodist is mixing up how it brings in innovative solutions to its team and patients is by taking its team outside of the Texas Medical Center and its hospitals in general. Now, Houston Methodist has a permanent tech hub in the Ion, owned and operated by Rice Management Company, on the lower level of the building, completely open to any of the Ion's visitors.
"We've always had a great partnership with Rice. This almost felt like an extension with Houston Methodist and our Rice collaboration with the Ion," Stansbury says. "Our main goals have been how can we utilize the talent that's housed out of that facility."
She explains that the new hub is an extension of the original hub in the TMC hospital, and that innovators who are interested in collaborating with Houston Methodist — especially those with solutions applicable to health care — can visit the Ion hub as an entry point.
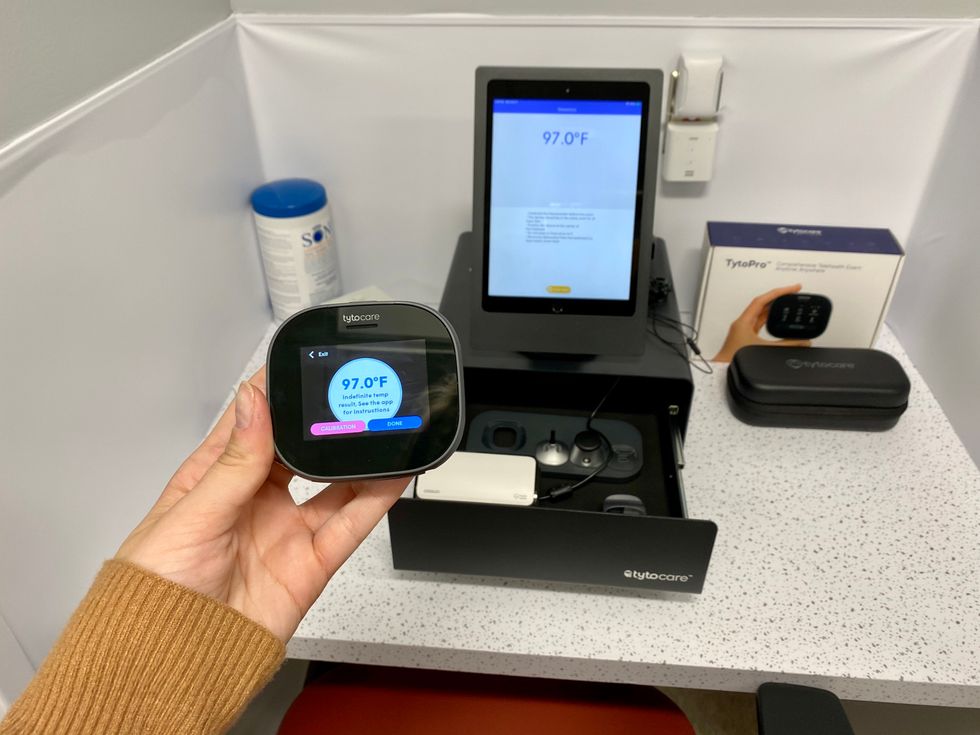
Both hub locations showcase pilot technology Houston Methodist is working on, and that technology will then get deployed out into its hospital locations — and especially its Cypress hospital, which is being billed as being the "smart hospital of the future." The construction is underway and expected to deliver in 2025.
Stansbury shares more about this ninth location for Houston Methodist as well as more details on the new tech hub on the podcast. Listen to the interview here — or wherever you stream your podcasts — and subscribe for weekly episodes.
- Houston hospital system to open new innovative location ›
- Houston Methodist boosts new Woodlands program thanks to $10M anonymous gift ›
- Houston hospital uses AI to create new breast cancer risk calculator ›
- Houston Methodist reveals details of new $1.4B tower ›
- Houston hospital introduces first-of-its-kind voice technology into its operating rooms ›
- Houston health tech leader to expand accelerator to continue connecting female founders - InnovationMap ›