The COVID-19 pandemic has had a drastic effect on every industry throughout the world. Additionally, we have all experienced multiple changes to our daily routine such as schools implementing virtual and hybrid learning while reconfiguring classrooms to promote social distancing and fitness studios closing off every other cardio machine and bench.
But no industry has had to pivot and innovate more than health care, which has been ground zero for the pandemic.
The pace of innovation for hospitals has been at breakneck speed — from the evolution of new treatment protocols to the need to reconfigure physical spaces to support an influx of patients while also promoting a healing environment during this unprecedented time.
Hospitals look and feel a lot different today because of significant modifications that have been made to care for patients and limit exposure to the virus. While a number of these modifications occurred under temporary state waivers, some of these changes may be here to stay.
Adding windows and alternative communication options to every room
Hospitals found that every room is valuable during a pandemic. Identifying and converting any available space, including private rooms like offices, break rooms, and conference rooms, was essential to accommodate an influx of patients during a surge. And when dealing with a highly infectious area, it is imperative to maximize staff and physician efforts while also safely minimizing the amount of time that staff members enter and exit rooms.
One way to do this is by adding windows in doors to promote patient visibility. This increased visibility can improve patient safety while conserving critical personal protective equipment. However, a down side to limiting the amount of times staff members enter and exit rooms is reduced valuable communication opportunities, which is why alternative mechanisms to communicate with patients must be in place in addition to increased visibility.
Implementing additional negative pressure capabilities
Like adding windows to every patient door, negative pressure rooms exist to keep non-contaminated areas free of airborne pathogens. In a negative pressure room, the air in the room is pulled into a room instead of being pushed out of a room, which is very effective in preventing airborne contaminants from escaping the room and infecting other people. But hospitals are not traditionally built with significant numbers of negative pressure rooms as demand for these types of rooms has historically been low.
In addition, the traditional way to design a facility is to spread negative pressure rooms throughout the hospital instead of consolidating them onto specific units. Although not required for COVID-19 patients, negative pressure rooms are helpful in ensuring maximum capabilities within different zones. In instances where negative pressure rooms could not be created, HEPA filters can still be used to "scrub" the air.
Converting anesthesia machines to ventilators
Anesthesia machines are capable of providing life-sustaining mechanical ventilation to patients with respiratory failure from diseases like COVID-19. They are used for this purpose every day in the operating room. Although they are not recommended for long-term ventilator needs, anesthesia ventilators can be modified to provide ventilatory support and are an obvious first-line backup when there are not sufficient ICU ventilators to meet patient care needs.
Building barriers to increase the safety of care
Plexiglass barriers have become a common sight in daily life including the front desks at hospitals. However, hospitals have taken it a step further and have either built or sourced equipment such as intubation boxes, which can be used during the intubation process, which consists of placing a breathing tube into a patient's airway and then connecting it to a ventilator or anesthesia machine if the patient is having surgery. Intubations are often done by an anesthesiologist, intensive care or emergency room provider; however, traditionally we had not often dealt with highly-contagious patients, so providing a higher level of protection is an important step in the containment of this type of virus.
The way healthcare providers enter and exit a COVID patient's room is as important as the proper use of PPE. In a pre-pandemic world, hospitals didn't specifically create spaces or areas within patient floors for staff to remove and discard their PPE and there wasn't any visible signage warning them that they were about to enter or leave a high-risk area. Many hospitals across the country have implemented color-coded zones within their COVID floors to caution staff of the type of precautions they should be taking at any given time. The creation of zones helps to protect staff and reduce contamination opportunities within the unit itself. Red, yellow and green zones using visual markers can be created to help provide staff designated areas that certain processes must be followed such as where PPE must be worn, where it can be donned and doffed and where PPE should not be worn.
Managing complex logistical challenges
Hospitals have been challenged with having to continue to provide uninterrupted care for COVID and non-COVID patients during the pandemic, while also handling, storing and administering vaccines. Hospitals have been at the forefront of the vaccine distribution system, working closely with state and federal officials to distribute vaccines on a large scale and reach the underserved populations that were hit hardest by COVID-19. For example, Baylor St. Luke's chose Texas Southern University, located within the Third Ward of Houston, as a vaccine site to reach communities of color and leverage its accessible location and the school's pharmacy students and faculty. And more recently, the hospital worked with Rice University to administer vaccines at its football stadium, a large venue that can be accessed easily through public transportation. Having these offsite venues with ample space has helped alleviate the space burden on hospitals during the vaccination efforts. Non-traditional healthcare delivery locations like these allow health care providers to administer more doses, closer to targeted communities than would be possible at a single hospital.
As we enter year two of the pandemic, the way hospitals function now and in the future is forever changed. Hospitals continue to learn and adapt during the COVID-19 pandemic, and in case of another pandemic, hospitals are better equipped to quickly pivot to provide care for a surge of patients and to assist in the recovery efforts.
------
Liz Youngblood is president of Baylor St. Luke's Medical Center and senior vice president and COO of St. Luke's Health.
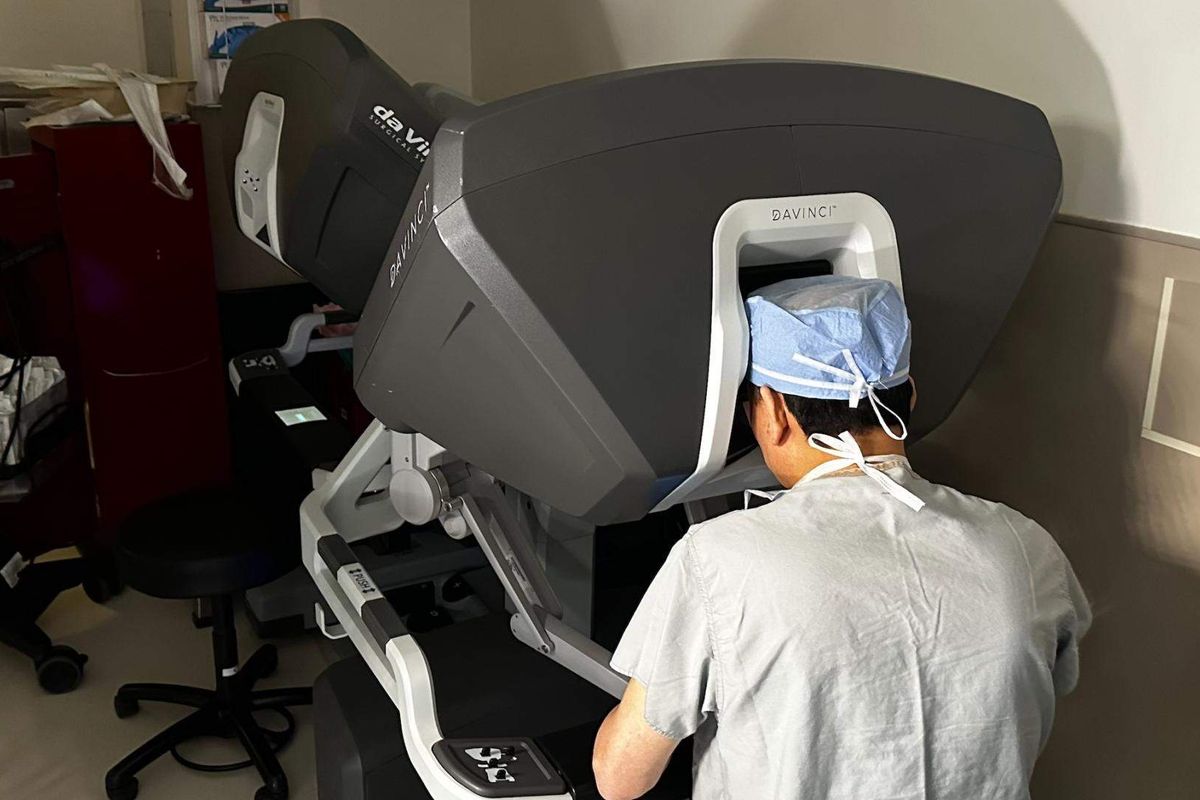






 Houston cardiac surgeon outpaces much of the country in game-changing robotics
Houston cardiac surgeon outpaces much of the country in game-changing robotics

 Apple doubles down on Houston with new production facility, training center Photo courtesy Apple.
Apple doubles down on Houston with new production facility, training center Photo courtesy Apple.