These 3 Houston research projects are revolutionizing health science
Research roundup
Researchers across the world are coming up with innovative breakthroughs regarding the coronavirus, but Houston research institutions are also making health and wellness discoveries outside of COVID-19.
Here are three from Houston researchers from a muscular atrophy study from outer space to a research project that might allow blind patients to "see."
Houston Methodist's research on muscular atrophy in astronauts

Scientists are studying the effect of certain drugs to help preserve muscles in astronauts. Photo courtesy of Houston Methodist/Facebook
Houston Methodist researcher Alessandro Grattoni and his team published research on muscular atrophy in astronauts. The research was published in Advanced Therapeutics and focused on his 2017 RR-6 muscle atrophy study that was conducted on the International Space Station.
While the current standard practice for astronauts maintaining their muscles is working out over two hours a day, the research found that use of drugs could also help preserve muscles. On a SpaceX refuel mission, mice that were implanted with a "Nanofluidic Delivery System" were sent up to space and monitored, according to a report. The device gradually released small doses of formoterol, an FDA approved drug for use in bronchodilation that has also been shown to stimulate increased muscle mass.
University of Houston researcher tracking fear response to improve mental health treatment

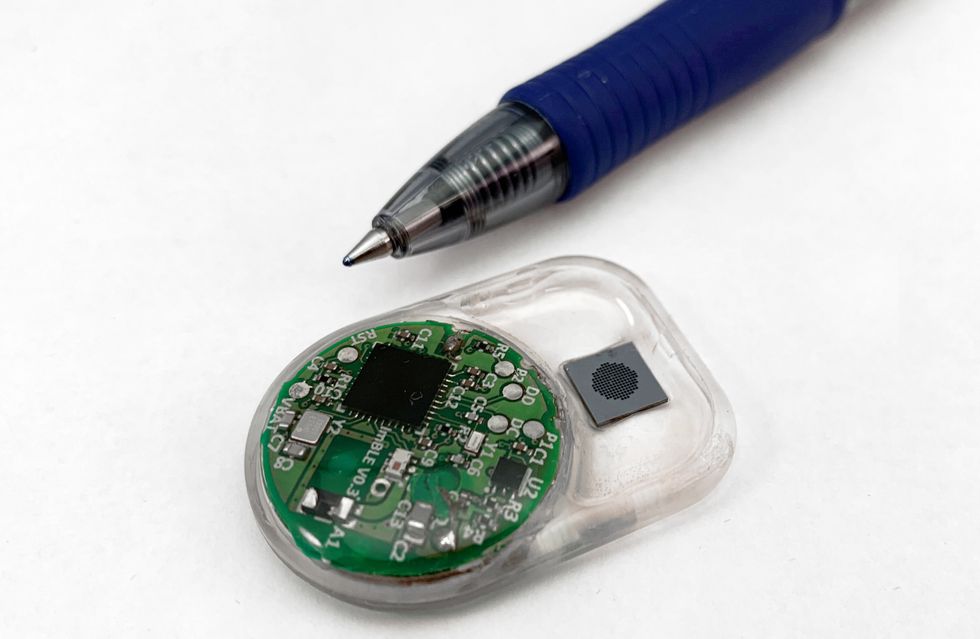
The research could help advance wearable devices. Photo via uh.edu
University of Houston researchers are looking into the way the body responds to fear in order to enhance mental health treatment. Rose Faghih, assistant professor of electrical and computer engineering, and doctoral student Dilranjan Wickramasuriya in the Computational Medicine Lab (CML) are leading the project.
"We developed a mixed filter algorithm to continuously track a person's level of sympathetic nervous system activation using skin conductance and heart rate measurements," writes Faghih in the journal PLOS One. "This level of sympathetic activation is closely tied to what is known as emotional arousal or sympathetic arousal."
When this sympathetic nervous system is activated — sometimes known as the "fight or flight" response — the heart beats faster and more oxygen is delivered to the muscles, according to a press release. Then, the body begins to sweat in order to cool down.
"Using measurements of the variations in the conductivity of the skin and the rate at which the heart beats, and by developing mathematical models that govern these relationships, CML researchers have illustrated that the sympathetic nervous system's activation level can be tracked continuously," reports Faghih.
This algorithm could be used in a wearable electronic device that could be worn by a patient diagnosed with a fear or anxiety disorder.
Baylor College of Medicine's vision-restoring research

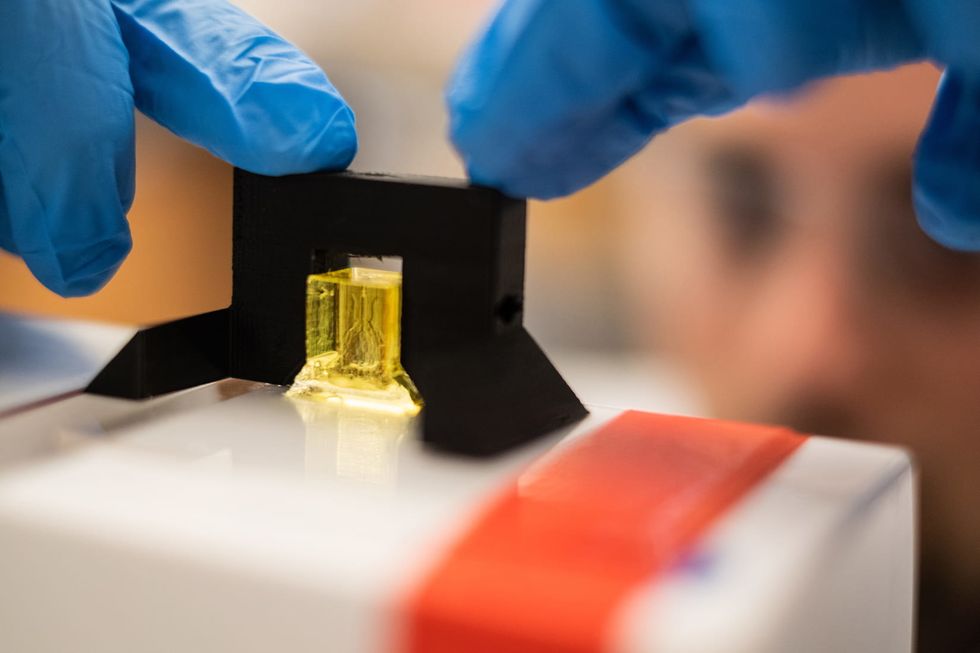
What if a device could see for you? Photo from Pexels
When someone loses their vision, it's likely due to damage to the eyes or optic nerve. However, the brain that interprets what they eyes sees, works perfectly fine. But researchers from Baylor College of Medicine have worked on a thesis that a device with a camera could be designed and implemented to do the seeing for the blind patient.
"When we used electrical stimulation to dynamically trace letters directly on patients' brains, they were able to 'see' the intended letter shapes and could correctly identify different letters," says Dr. Daniel Yoshor, professor and chair of neurosurgery in a press release. "They described seeing glowing spots or lines forming the letters, like skywriting."
Through a study supported by the National Eye Institute with both sighted and blind people using implanted devices, the investigators determined that the process was promising. According to the release, the researchers identified several obstacles must be overcome before this technology could be implemented in clinical practice.
"The primary visual cortex, where the electrodes were implanted, contains half a billion neurons. In this study we stimulated only a small fraction of these neurons with a handful of electrodes," says said Dr. Michael Beauchamp, professor and in neurosurgery, in the release.
"An important next step will be to work with neuroengineers to develop electrode arrays with thousands of electrodes, allowing us to stimulate more precisely. Together with new hardware, improved stimulation algorithms will help realize the dream of delivering useful visual information to blind people."