Rice, MD Anderson receive $1.5 million to further brain cancer research
fresh funding
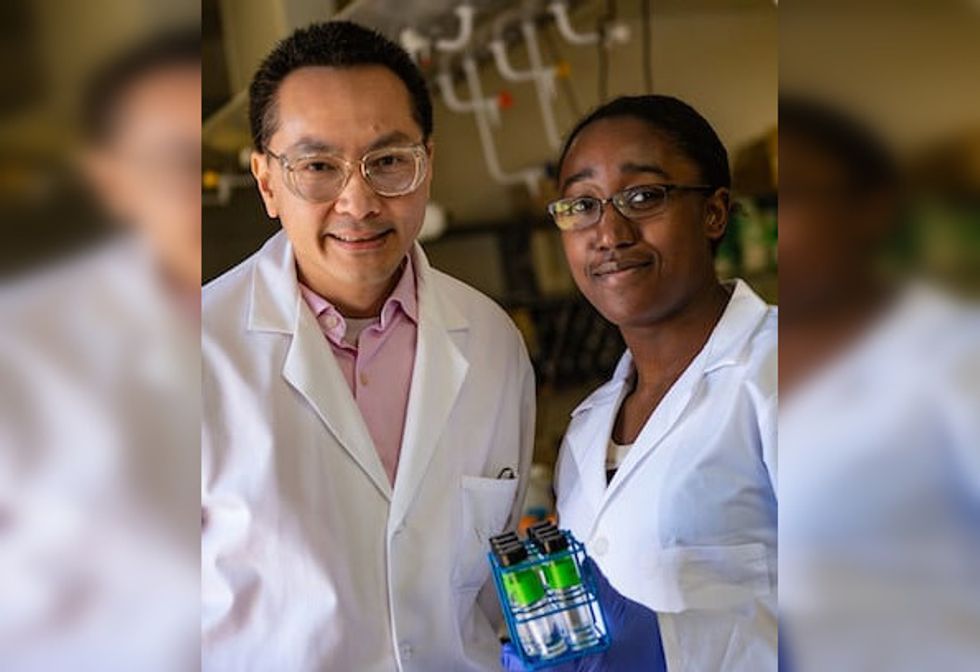
Rice University chemist Han Xiao, who also serves as director of the university’s Synthesis X Center, and cancer biologist Dihua Yu of The University of Texas MD Anderson Cancer Center have received a three-year, $1.5 million grant from the Robert J. Kleberg Jr. and Helen C. Kleberg Foundation.
The funding will allow them to continue their research on treating brain metastasis by overcoming the blood-brain barrier, or the BBB, according to a news release.
Brain metastasis is the leading form of brain cancer, with survival rates below 20 percent within a year of diagnosis, according to the National Library of Medicine. It commonly originates from breast, lung and melanoma cancers.
The BBB typically acts as a protective barrier for the brain. However, it prevents most drugs from being able to directly reach the brain. According to Rice, only 2 percent of FDA-approved small molecule drugs can penetrate the BBB, limiting treatment options.
Xiao and Yu’s approach to dealing with the BBB includes a light-induced brain delivery (LIBD) platform. The advanced system employs nanoparticles that are embedded with a near-infrared dye for the transport of therapeutic agents across the BBB. The research will evaluate the LIBD’s ability to improve the delivery of small-molecule drugs and biological therapies. Some therapies have shown potential for reducing cancer growth in laboratory studies, but they have struggled due to limited BBB penetration in animal models.
“Our LIBD platform represents a novel strategy for delivering drugs to the brain with precision and efficiency,” Xiao said in a news release. “This technology could not only improve outcomes for brain metastasis patients but also pave the way for treating other neurological diseases.”
The Kleberg Foundation looks for groundbreaking medical research proposals from leading institutions that focus on “innovative basic and applied biological research that advances scientific knowledge and human health” according to the foundation.
“This research is a testament to the power of collaboration and innovation,” Xiao said in a news release. “Together, we’re pushing the boundaries of what’s possible in treating brain metastasis and beyond.”
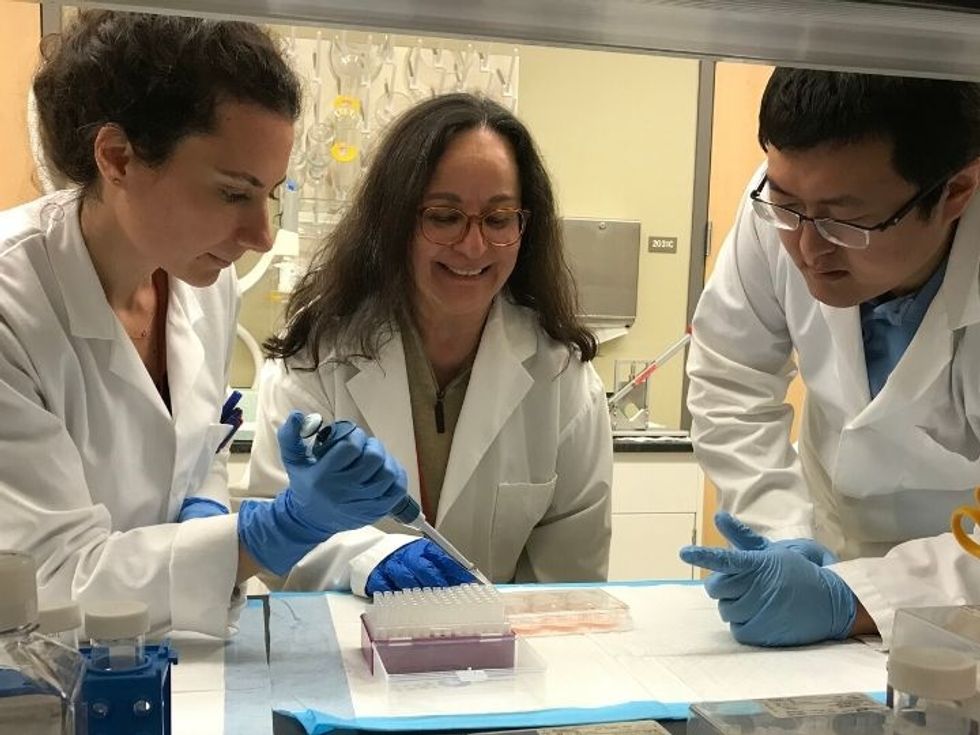
Rice launched the Synthesis X Center, or Synth X, last spring. It was born out of what started about eight years ago as informal meetings between Xiao's research group and others from the Baylor College of Medicine’s Dan L Duncan Comprehensive Cancer Center. It aims to turn fundamental research into clinical applications through collaboration.
“This collaboration builds on the strengths of both research teams,” Xiao said in the release. “By combining SynthX Center's expertise in chemistry with Dr. Yu's expertise in cancer biology and brain metastases, we aim to create a transformative solution.”
- Texas nonprofit cancer research funder doles out millions to health professionals moving to Houston ›
- Houston organizations snag chunk of recently announced $49M cancer research grant funding ›
- Houston hospital names leading cancer scientist as new academic head ›
- UH research team receives grant to fight aggressive pediatric cancer ›
- Houston cell therapy company launches second-phase clinical trial - InnovationMap ›
- MD Anderson, TOPPAN launch joint venture for invivoid cancer treatment tech - InnovationMap ›