Houston researchers advance unique nasal vaccine that prevents COVID transmission
cutting spread at the source
Since the force of COVID-19 hit globally in 2020, scientists have made efficient progress in the fight against it. As Dr. Navin Varadarajan puts it, vaccines have “allowed us to become a society again.”
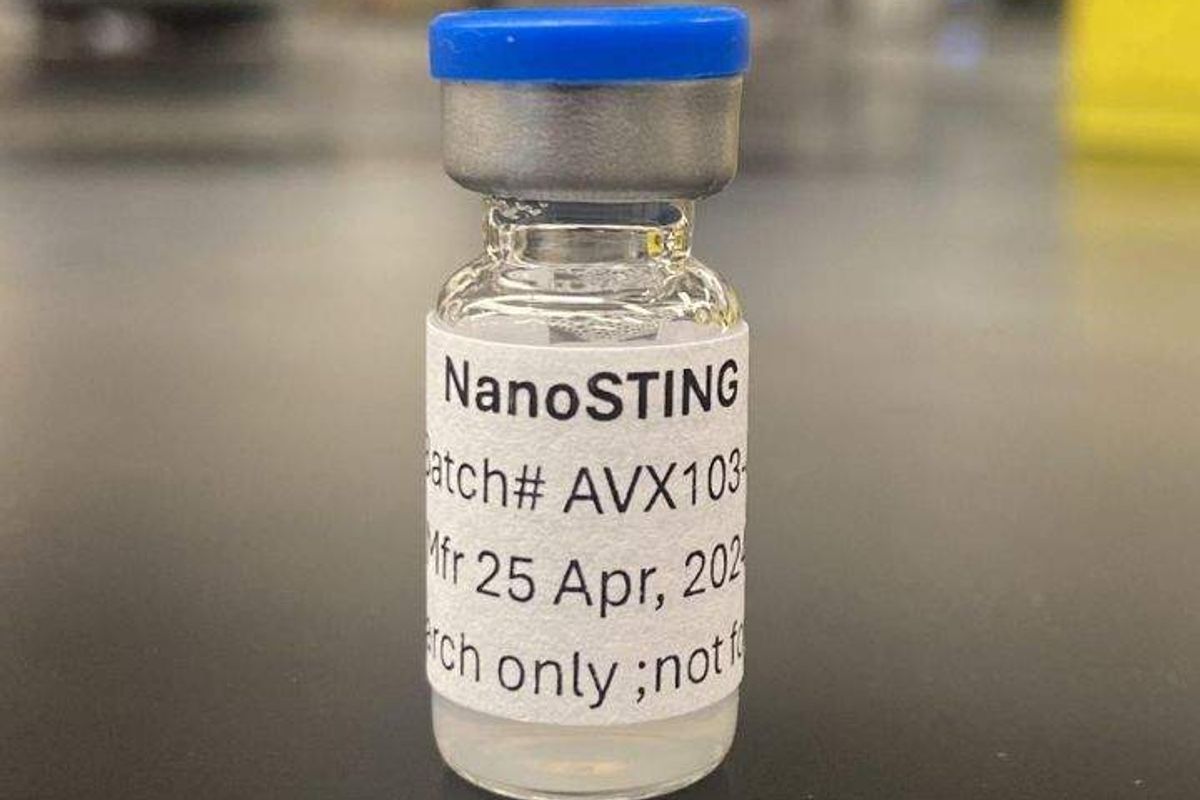
And he should know, the M.D. Anderson Professor of William A. Brookshire Chemical and Biomolecular Engineering at University of Houston just published back-to-back studies for nasal sprays that combat viruses. One, the NanoSTING therapeutic, has proven effective in treating strains of SARS-CoV-2 and the flu virus. The other, NanoSTING-NS Pan-coronavirus Vaccine is targeted at preventing the transmission of multiple COVID variants altogether.
Why a nasal vaccine? Varadarajan explains that while COVID vaccines prevent advanced disease, they don’t prevent transmission.
“Intramuscular vaccines do not facilitate a component of peer immunity called mucosal immunity, which takes care of these points of entries, these wet surfaces, which can be of the nose and the wet surfaces of the nose, and so they don't prevent transmission,” he tells InnovationMap. “So I can be vaccinated, I pick up a small infection that's confined largely to my nostrils, and I can still pass it on to vulnerable people, the aged, the immunocompromised people who have all the drugs they're taking to fight other things, like cancer patients. And so for them, the vaccines tend to be less efficacious, and if I transfer it to them, unfortunately they can end up in a hospital, right? And so preventing transmission is the way to end this cycle.”

The NanoSTING-NS is also notable for its potential ability to end what Varadarajan calls “the endless cycle of boosting.” The way to do that, he explains, is to prevent the infection at its root. And theoretically, his lab’s invention could do that. But he cautions readers not to get too excited just yet.
The vaccine is currently in the phase of animal testing, though Varadarajan is hopeful that it could move to human samples in about a year.
The therapeutic can treat multiple respiratory viruses by using fat droplets to deliver the immune booster cGAMP.
“The ability to activate the innate immune system presents an attractive route to armoring humans against multiple respiratory viruses, viral variants and also minimizing transmission to vulnerable people,” says postdoctoral associate Ankita Leekha, first author on the paper that shares NanoSTING’s findings. “The advantage of NanoSTING is that only one dose is required, unlike the antivirals like Tamiflu that require 10 doses.”

Varadarajan puts it even more simply: “Just like we have Tylenol, just like you take aspirin, you feel like you have some symptoms, and you take it afterwards.”
Currently, he says that the partners with whom the lab is working towards commercialization are prioritizing the therapeutic over the vaccine. The reasons are clear. Varadarajan explains that, while we’ve now long had antibiotics to broadly combat infections, there hasn’t been anything like that to battle viruses. With its ability to target multiple viruses, NanoSTING could be that innovation.
“We activate the innate immune system. So our drug is not virus-specific. Our drug works by activating your own immune system, and that will then fight off different kinds of viruses,” he says.
A single product that treats everything from the common cold to COVID-19 by capitalizing on the patient’s own immune system could be closer than we realize.
- University of Houston designs device that instantly kills COVID-19 ›
- Texas vodka brand doles out $1M grant to Houston research institution for COVID-19 vaccine ›
- Houston doctors get approval for low-cost COVID vaccine abroad ›
- How Houston ranks as global leader, digital health co. raises pre-seed, and more trending innovation news ›
- University of Houston researchers studying COVID-19 prevention and treatment ›
- University of Houston lab reports breakthrough in cancer-detecting technology ›

 Apple doubles down on Houston with new production facility, training center Photo courtesy Apple.
Apple doubles down on Houston with new production facility, training center Photo courtesy Apple.